Contrary to the medical marketing hype, synthetic hormonal drugs, dairy products and most calcium supplements actually weaken the bones and have other harmful effects on health.
 Osteoporosis is big news – and big business – these days. It emerged as a bona fide disease only three decades ago. Since then, it has been promoted to all menopausal women as a serious health concern that needs medical intervention.
Advertising campaigns in the media and fact sheets in doctors’ waiting rooms and pharmacies continually warn women of the dangers of disappearing bone mass. The solutions offer include pharmaceutical drugs, HRT, calcium supplements and a high dairy diet. But is osteoporosis really a devastating condition? And will the mainstream medical solutions for creating strong, resilient bones really support women to safely optimise bone health?
Behind so many of the recommended approaches that promise to ensure women’s strong bones, dwell many myths and misinformation.
Our Miraculous Bones
To understand the many myths about osteoporosis and its prescribed treatments, it is vital to first understand the nature of bones.
Bone is living tissue which undergoes constant transformation. Bone might appear to be static, but, in fact, as living tissue it is continuously being renewed. Bone, as living tissue, is constantly in a cycle of being broken down and reformed. This process is known as bone remodelling and requires an adequate supply of many nutrients. At any given moment in each of us, there are from 1 to 10 million sites where small segments of old bone are being dissolved and new bone is being laid down to replace it.
Bone tissue is nourished and detoxified by blood vessels in constant exchange with the whole body. Bone-forming cells are of two different kinds: osteoclasts and osteoblasts. The job of osteoclasts is to travel through the bone in search of old bone that is in need of renewal.
Osteoclasts dissolve bone and leave behind tiny unfilled spaces. Osteoblast cells then move into these spaces in order to build new bone. This self-repair capability is extremely important. Imbalances in bone-remodelling contribute to osteoporosis. When more old bone is eaten up than new bone is laid down, bone loss occurs.
Bone turnover never stops completely. In fact, after about the age of 50 the rate increases, although it’s not quite coordinated. The bone-building cells, the osteoblasts, become less and less capable of completely refilling the spaces made by the osteoclasts. The peak amount of bone you started with and the rate of this loss determines the density of your bones. Density varies greatly in different individuals, cultures, races and sexes.
 The medical definition of osteoporosis used to be “fractures caused by thin bones”. It has since been redefined to “a disease characterised by low bone mass and microarchitectural deterioration of bone tissue which led to increased bone fragility and a consequent increase in fracture risk.â€
The medical definition of osteoporosis used to be “fractures caused by thin bones”. It has since been redefined to “a disease characterised by low bone mass and microarchitectural deterioration of bone tissue which led to increased bone fragility and a consequent increase in fracture risk.â€
However, there is a problem with defining osteoporosis as a disease, not a risk of fracture. Low bone mass is only one risk-factor for osteoporosis, not osteoporosis itself. It’s a warning sign that might be useful, so you can begin to consider ways to keep the disease itself from occurring. It’s is like defining heart disease as having high cholesterol rather than having a heart attack. Needless to say, this new definition has increased the number of women and men who have osteoporosis.
Healthy bones have two components- bone density and micro-architecture. The problem is that, presently, only part of the bone health story is addressed – bone density.
The good news is that just because you may have with low bone density, it doesn’t mean that you will get a fracture. For instance, Asian women have low bone density, yet have very low rates of bone fractures. The general assumption has been that once a bone reaches a certain level of thinness; it will fracture more easily. But according to bone physiology, it is clear that this is not the full story. Bone don’t fracture due to thinness alone.
Osteoporosis by itself does not cause bone fractures. This is documented simply by the fact that half of the population with thin osteoporotic bones never fracture!
There is so much more to the osteoporosis story. Like so many aspects of our health, it is critically important to discern fact from fiction.
Menopause – A Mythical Cause of Osteoporosis
 There are many cultures in the world where the postmenopausal woman is fit, active and healthy until the end of her life. It is equally true that the women in these cultures do not suffer from osteoporosis. If menopause itself were indeed one of the causes of osteoporosis, all women throughout the world would be handicapped with fractures. This is clearly not the case.
There are many cultures in the world where the postmenopausal woman is fit, active and healthy until the end of her life. It is equally true that the women in these cultures do not suffer from osteoporosis. If menopause itself were indeed one of the causes of osteoporosis, all women throughout the world would be handicapped with fractures. This is clearly not the case.
The Mayan women live for 30 years after menopause, but they don’t get osteoporosis, they don’t lose height, they don’t develop dowager hump and they don’t get fractures. A research team analysed their hormone levels and bone density and found that their oestrogen levels were no higher than those of Caucasian American women. And in some cases, they were even lower. Bone density tests showed that bone loss occurred in these women at the same rate as their US counterparts. It used to be thought that all women have a considerable decrease in bone from lower oestrogen levels at menopause, thus oestrogen deficiency was said to be the cause of osteoporosis. Continuing research has disproved this idea.
Studies following individual women’s bone density over time have shown that although some women lose a lot of bone with menopause, others lose comparatively little; also, that some loss starts earlier. One study using urine tests to measure calcium loss found that some women are ‘fast losers’ and others are naturally ‘normal losers’. If osteoporosis is due to oestrogen deficiency alone, we would expect to find lower oestrogen levels in women with osteoporosis than in women without the disorder. However, studies have shown that sex hormone levels were found to be similar in postmenopausal women both with and without osteoporosis.
Obviously, it is a gross oversimplification to say that osteoporosis is a single, inevitable disease which occurs in all women at menopause. For instance, a woman who had her ovaries surgically removed had double the loss of bone compared to a woman going through a natural menopause. Since the ovaries continue to produce hormones in addition to oestrogen after menopause, it is obvious that oestrogen is only one factor connected to bone loss. Numerous dietary, lifestyle and endocrine factors contribute to the development of excessive bone loss. The intention to make menopause and oestrogen deficiency the major causes of osteoporosis gave Hormone Replacement Therapy new legitimacy as a long-term preventive treatment for osteoporosis. Even though oestrogen has been shown to have some effectiveness in slowing down the rate of bone loss because it slows the rate at which bone cells are resorbed, it cannot rebuild bone.
Unfortunately, this benefit is not experienced by all women. To have any effectiveness for the postmenopausal women most at risk-those 70 years of age or older-women must stay on oestrogen continuously for decades. This, then, becomes quite a serious dilemma for women. It is now known that HRT increases the incidence of breast cancer by 10 per cent a year for each year of use. Ten years of taking HRT increases the risk to 100 per cent. It is obvious that the many risks of HRT far outweigh the rather limited beneficial effects on bone, especially when there are many other safe and effective alternatives. Is the increased risk of a life-threatening disease really worth it?
The Calcium Deficiency Myth
When asked about the causes of osteoporosis, most people will chime in with “Lack of calcium”. This idea is reinforced on a daily basis as women are reminded to drink their three glasses of milk a day and take their calcium supplements.
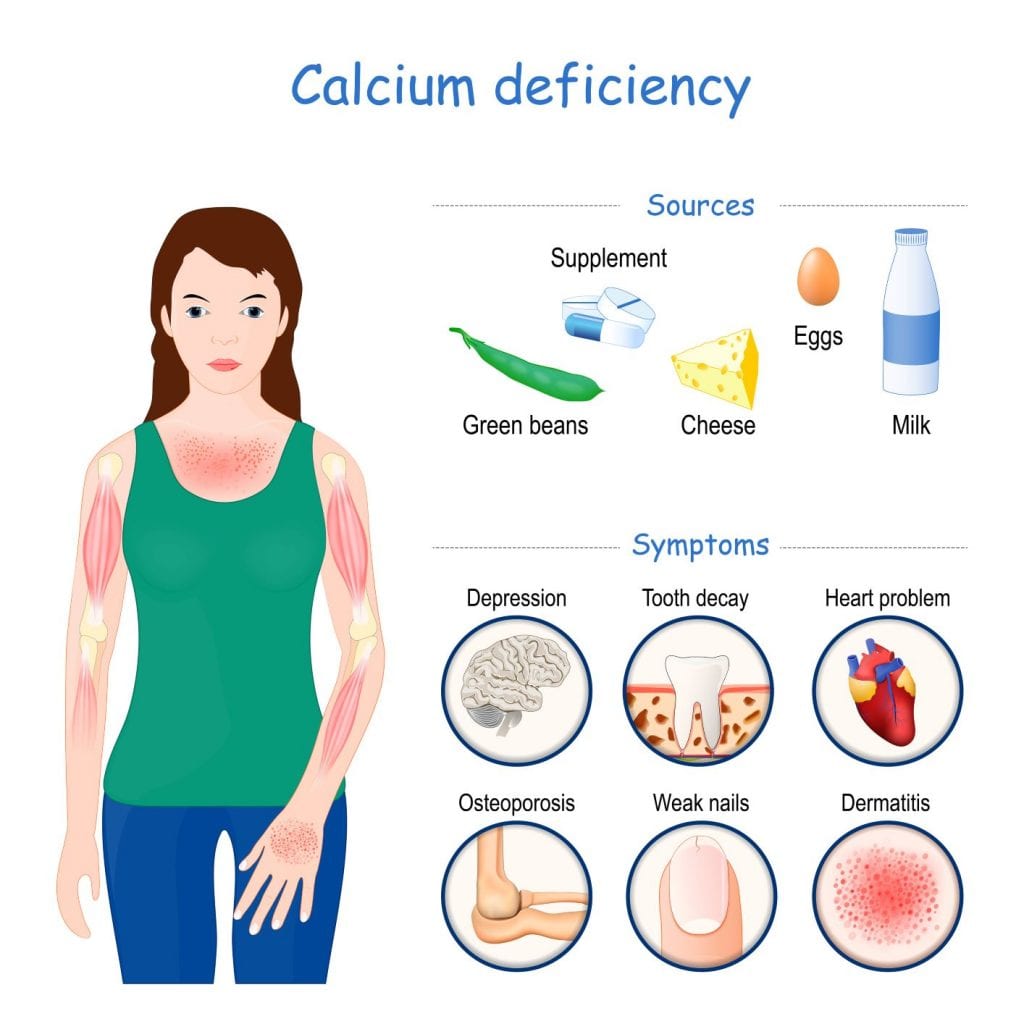
Even young, healthy, non-osteoporotic women are paranoid about potential bone loss and take measures to shore up their bone strength with plenty of calcium. Fear of insufficient calcium has become a national obsession.
Is there really a national calcium deficit?
Since bone is largely composed of calcium, it might appear logical to link calcium intake with bone health. Western women are now encouraged to consume at least 1,000 to 1,500 mg of calcium daily. It is curious, however, when cross-cultural data clearly shows that in less-developed countries-where people consume little or no dairy products and ingest less total calcium-there are much lower rates of osteoporosis. The Bantu of Africa have the lowest rates of osteoporosis of any culture, yet they consume from 175 to 476 mg of calcium daily. The Japanese average about 540 mg daily, but the early postmenopausal spinal fractures, so common in the West, are almost unheard of in Japan. Overall, their spinal fracture rate is one-half that of the US. All this is true, even though the Japanese have one of the longest life spans of any population. Studies of populations in China, Gambia, Ceylon, Surinam, Peru and other cultures all report similar findings of low calcium intake and low osteoporosis rates. While it is agreed upon that adequate calcium is absolutely necessary for development and maintenance of healthy bones, there is no one standard ideal calcium intake. It is also obvious from these studies that high calcium intake is not necessary for healthy bones.
The body uses minerals only when they are in proper balance. For example, girls who consume diets high in meat, soft drinks and processed foods which have high levels of phosphorus have been found to have an alarming loss of bone mass. Too high a ratio of phosphorus in relationship to calcium will cause calcium to be pulled out of the bones in an attempt to compensate.
Scientific evidence shows unequivocally that, by themselves, calcium supplements just don’t work. And contrary to popular thought, calcium supplementation does not reduce the risk of fracture. There is now evidence that a high calcium supplement level is actually associated with a 50 per cent increase in the risk of fracture.
However, as yet, there remains no proof that increasing the calcium intake with supplements or diet after menopause prevents fractures. In fact, several studies indicate that it doesn’t really appear to lower the incidence of fractures at all.
In the journal, Science, it was stated the “link between calcium and osteoporosis was made on insufficient grounds” and that the advertisers were way out ahead of the scientific evidence. But it is true that a diet rich in natural sources of calcium-rich foods, such as green-leafy vegetables, sardines and salmon, seeds, cheese, yoghurt, beans, lentils and almonds, eaten in early childhood and pre-menopausal years helps to build stronger bones, reducing risk of thin bones after menopause.
The worst calcium supplements are bone meal, oyster shell, dolomite and calcium carbonate because they cannot be efficiently absorbed and may contain lead. Excessive calcium intake also leads to constipation and, more worrisome, kidney stones, breast cysts and calcification of the joints.
The most effective form of calcium supplementation is hydroxyapatite (especially if it is formulated with boron). This is the most natural of all calcium supplements and a complete bone food. If you want healthy bones, it is important to include additional proven bone building nutrients such as magnesium, a compressive multi-mineral supplement, Vitamin D, Vitamin K2, omega fatty acids, and protein. Here’s the truth. You can rebuild bone density and create healthy bone naturally at any age!
Stay tuned for Part 2 of The Myths and Truths About Bones
 Sherrill Sellman, N.D., Naturopathic Doctor (Board Certified in Integrative Medicine), is an educator, women’s natural health expert, psychotherapist and journalist in the field of women’s health. She is also, a much sought-after international lecturer, host of two women’s weekly radio shows, senior editor and contributing writer to numerous health publications. Dr. Sellman is the best-selling author of Hormone Heresy: What Women MUST Know. She is the formulator of Hygeena, a comprehensive natural formula for vaginal dryness. Her website is drsherrillsellman.com.
Sherrill Sellman, N.D., Naturopathic Doctor (Board Certified in Integrative Medicine), is an educator, women’s natural health expert, psychotherapist and journalist in the field of women’s health. She is also, a much sought-after international lecturer, host of two women’s weekly radio shows, senior editor and contributing writer to numerous health publications. Dr. Sellman is the best-selling author of Hormone Heresy: What Women MUST Know. She is the formulator of Hygeena, a comprehensive natural formula for vaginal dryness. Her website is drsherrillsellman.com.
References:Â
-
Love, Susan, MD, Dr Susan Love’s Hormone Book, Random House, New York, 1997
Colditz, G. A. (1998), -
“Relationships between estrogen levels, use of hormone replacement therapy and breast cancer”,
-
J. NCI 90(11):814-823. Brown, Susan, PhD, Better Bones, Better Body, Keats Publishing, Connecticut, USA, 1996
-
Melton, L. and B. Riggs, “Epidemiology of Age-related Fractures”, in The Osteoporotic Syndrome: Detection, Prevention and Treatment (L. Avioli, ed.), Grune & Stratton, New York, 1983
-
Robert Cohen’s website, <www.notmilk.com>.
-
Colgan, M., Dr, The New Nutrition, Apple Publishing, Canada, 1995
-
Beckham, Nancy, Natural Therapies for Menopause and Osteoporosis, published by Nancy Beckham, NSW, Australia, 1997